Key Takeaways
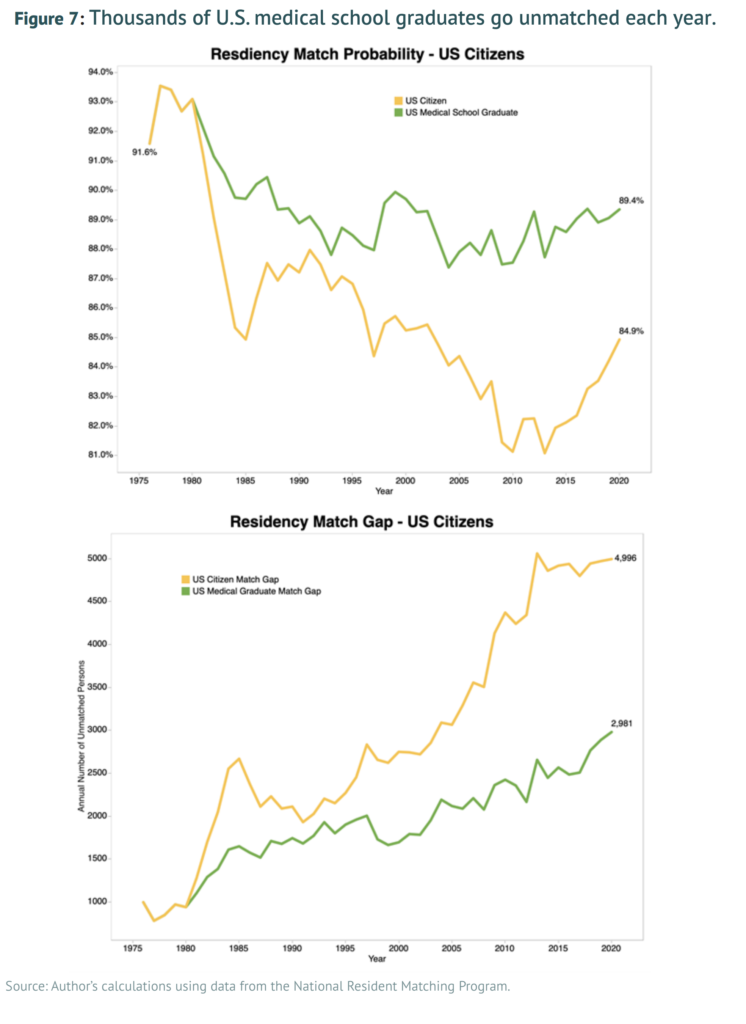
- The residency system is the primary bottleneck in the pipeline for training U.S. physicians, limiting the supply of doctors and thus access to medical services.
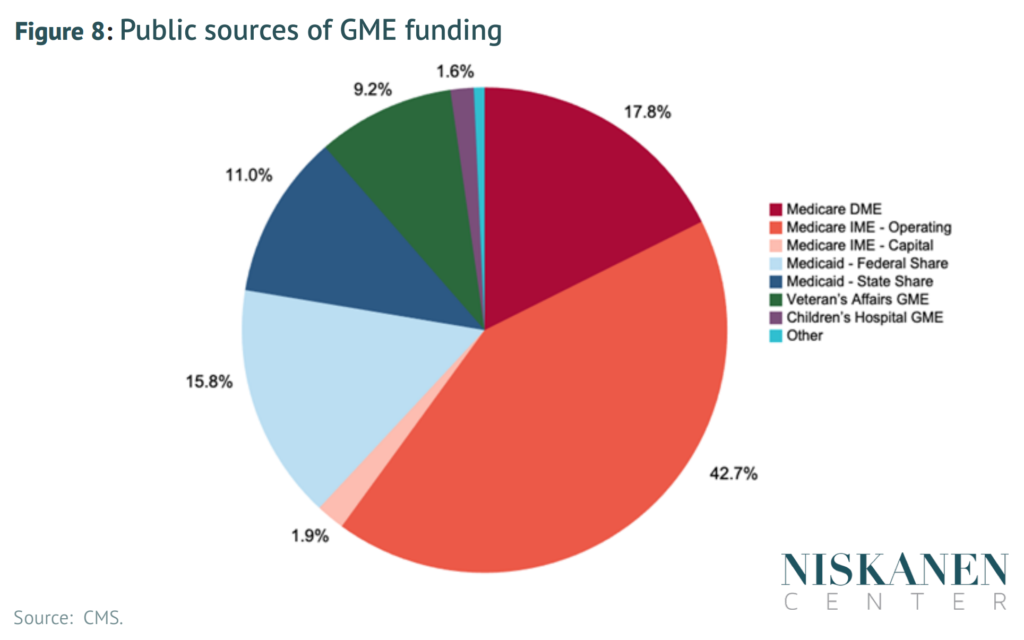
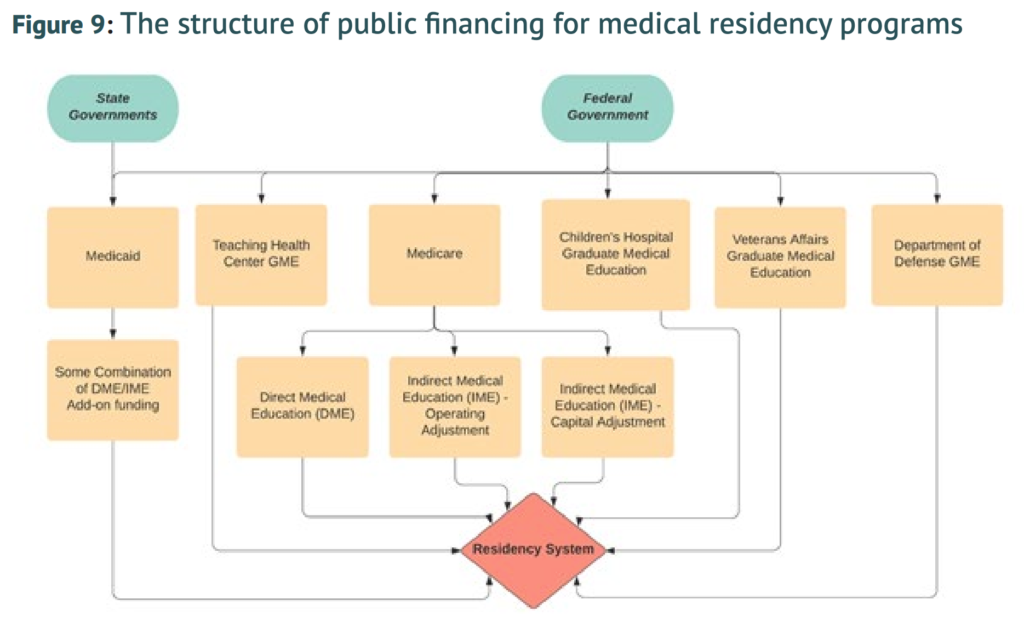
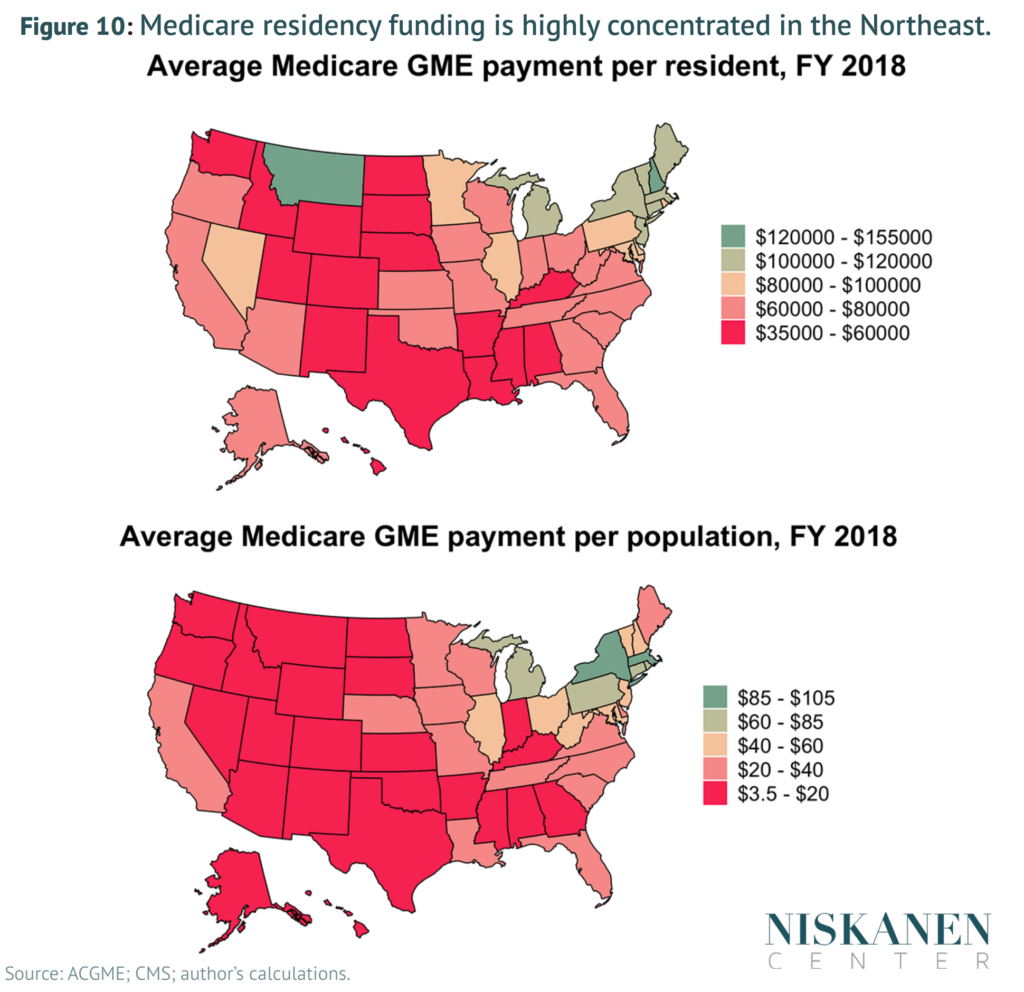
- Current federal funding for graduate medical education is inefficient and inequitable, severely limiting the effectiveness of present subsidy schemes. Simply increasing funding without enacting structural reforms will do little to address the physician-supply bottleneck.
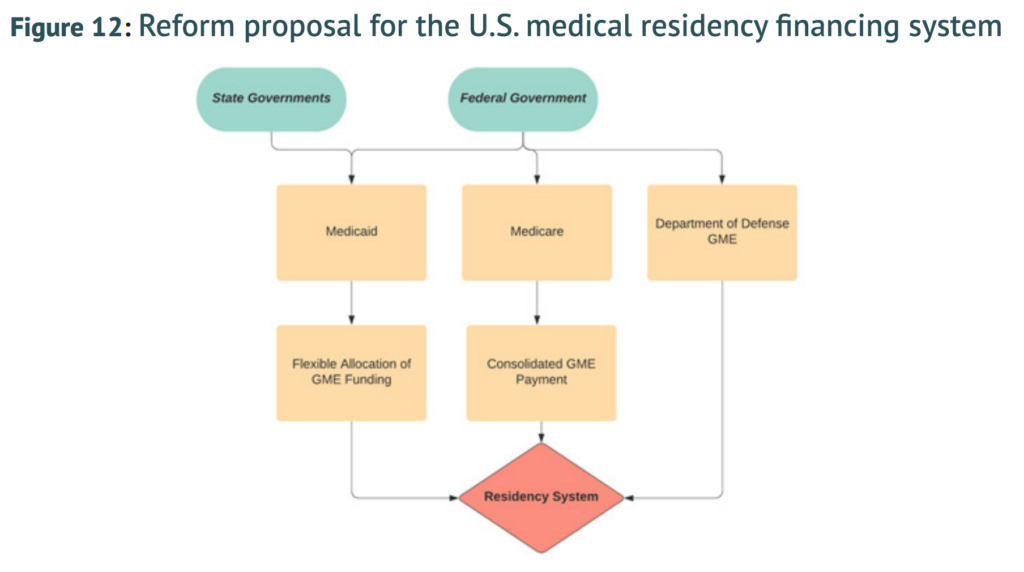
- Funding streams to hospitals for graduate medical education should be consolidated and modernized in order to efficiently train U.S. physicians where they are needed most.
- Congress should update current Centers for Medicare & Medicaid Services (CMS) rules on federal matching for Medicaid GME, granting states greater freedom to strategically target the financing.
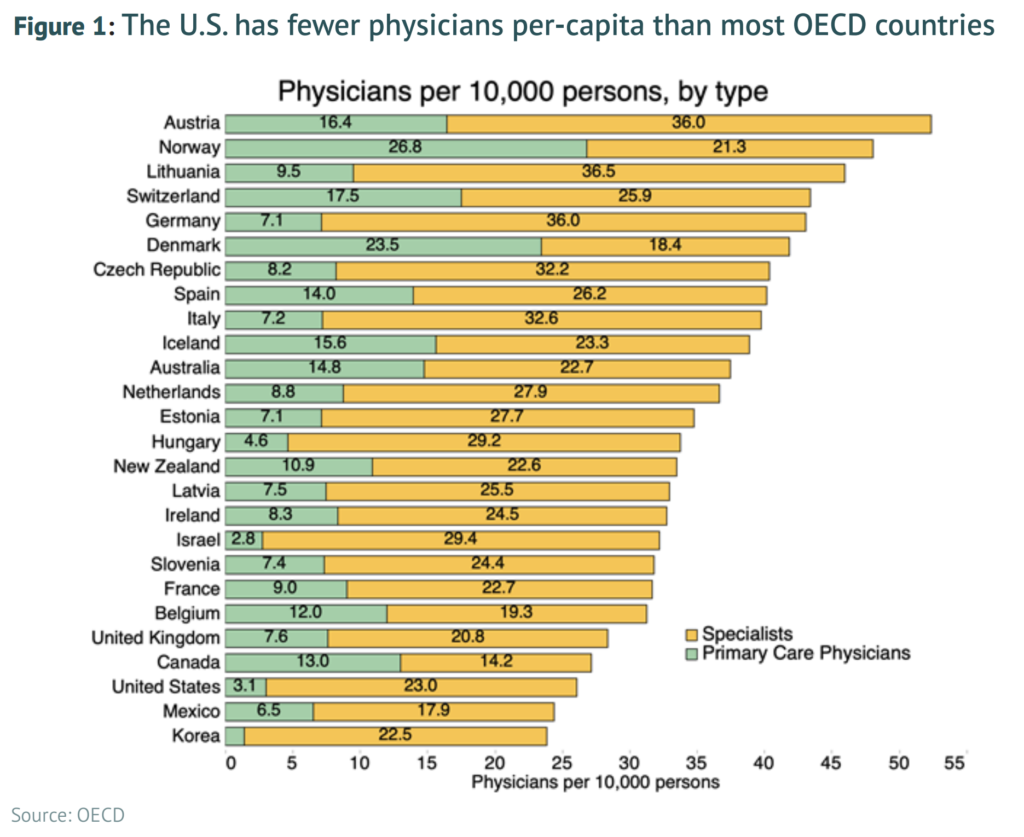
Physicians are the cornerstone of any health care delivery system. Nonetheless, the United States employs substantially fewer of these professionals than most other developed countries. Given that the number of physicians per person is a reasonable proxy for the number of service access points within a health system, the United States therefore faces greater challenges in delivering basic, accessible care to its citizens compared to other developed countries.
At the most abstract level, this lack of physicians is a puzzle. The combined cost of a medical degree and postgraduate residency training is many multiples smaller than the expected lifetime earnings of those who complete residency and become a licensed physician. This raises the question: If the financial incentives are there, why do we have so few doctors?
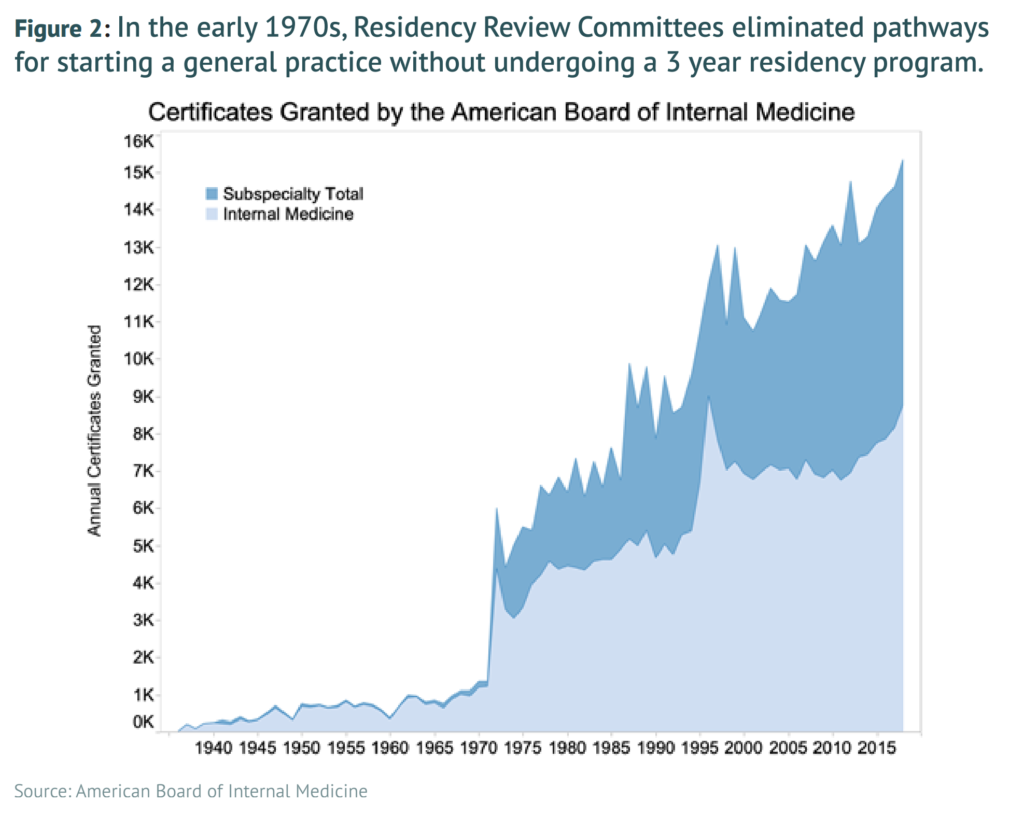
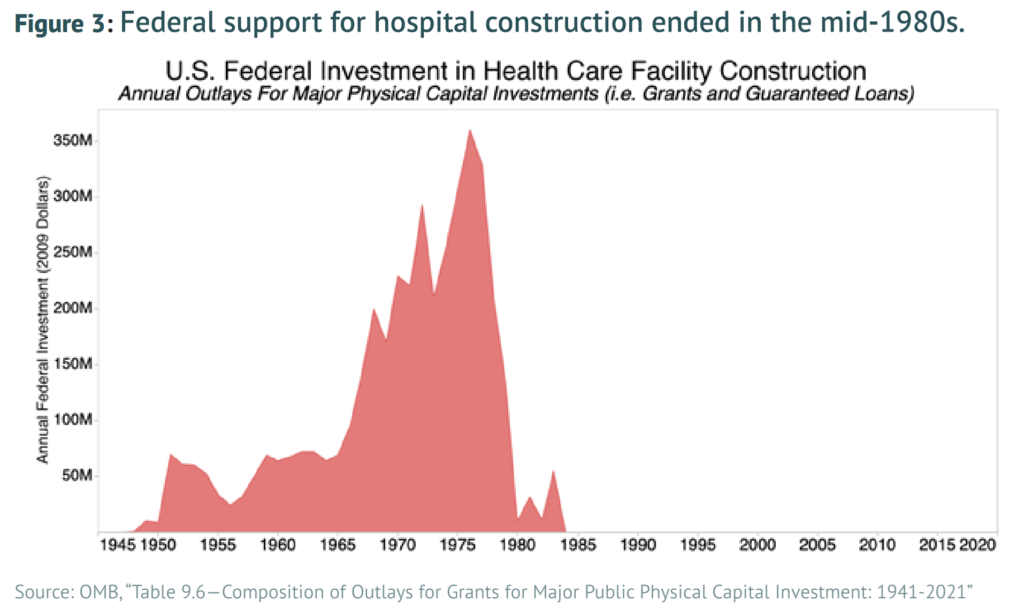
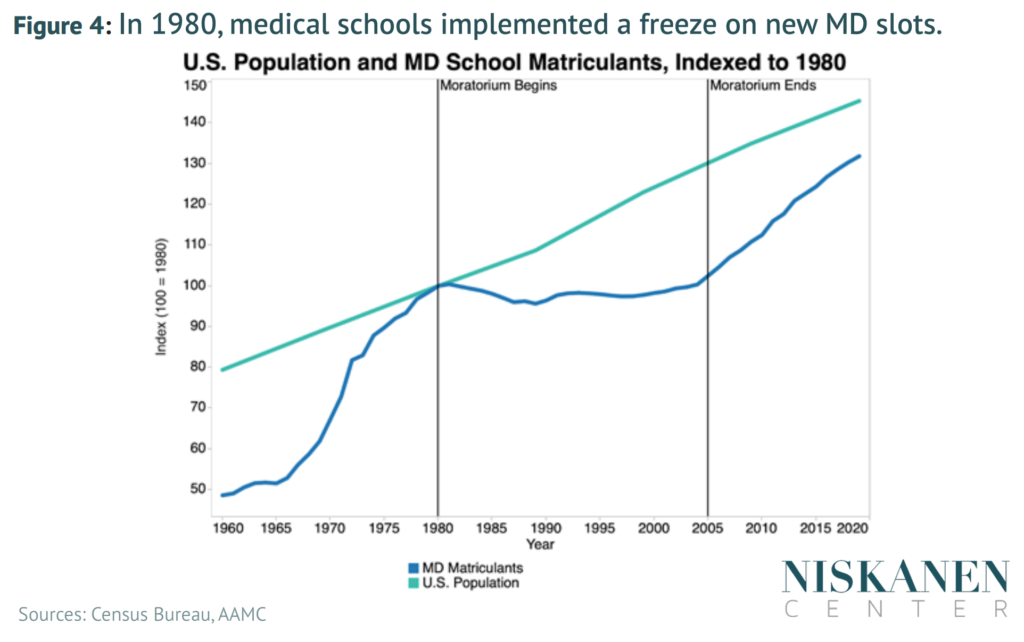
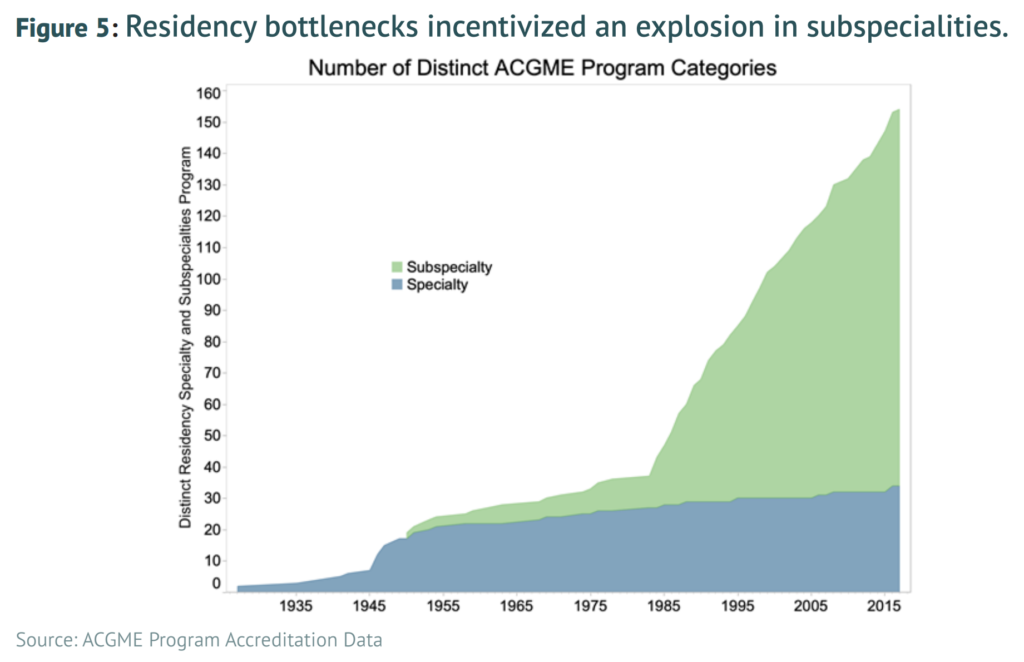
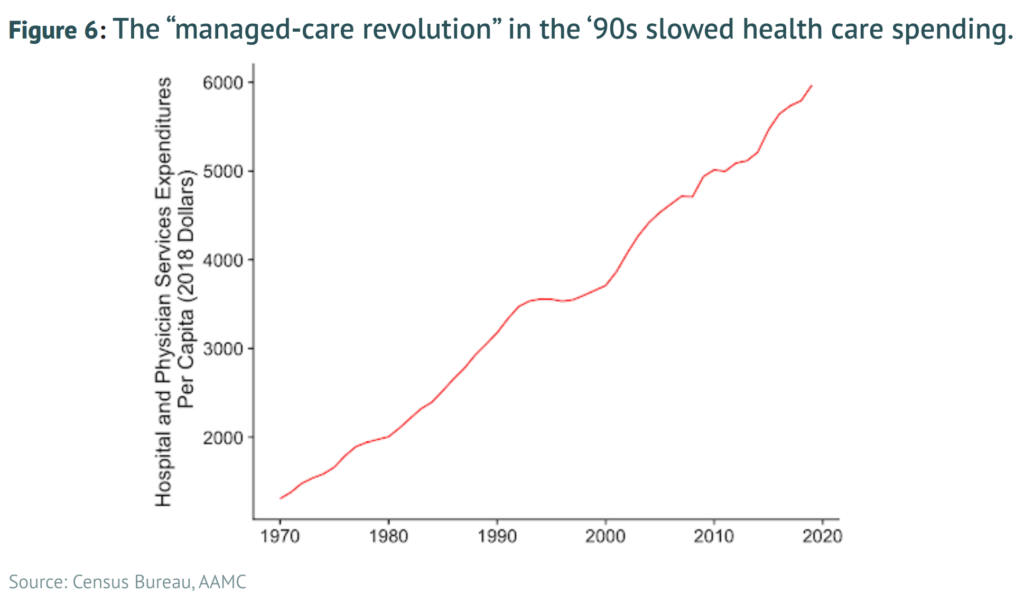
The key reason for our physician shortfall is that substantial bottlenecks exist in the training and education pipeline, with the most significant of these being the medical residency system. These bottlenecks were initially encouraged by policymakers based upon the misguided belief that limiting physician supply would control rising health care costs. Yet these attempts to constrain physician supply growth beginning in the 1980s have been an utter policy failure, leading to no noticeable reduction in health care costs. Because physicians are the U.S. health care system’s primary access point, the health system has effectively been encouraged to pursue high-intensity, low-access care. The United States thus has little to lose and much to gain from increasing the supply of physicians across the board, which will require reforming and modernizing federal support for the physician residency system.
Click here to read the full report.
Figures
Click to enlarge.

Robert Orr is a Policy Analyst at the Niskanen Center