September has been an incredibly exciting time for those working on drug pricing and intellectual property. Not only did this month mark the tenth anniversary of the America Invents Act, but it also saw the release of three key documents signaling a sea change in how the United States will handle the issue of drug pricing, with a special focus on intellectual property.
These three documents, a report from the Department of Health and Human Services, a letter to the acting Patent and Trademark Office director from the Food and Drug Administration, and a letter from the heads of the Senate Intellectual Property Subcommittee, are each worth going over in detail. They cover similar topics and sometimes discuss the same specific issues. Examined holistically, these communications are milestones on a serious
In July, President Biden signed his executive order ““Promoting Competition in the American Economy.” The EO was a wish list of reforms to promote competition, and a significant portion of it focused on issues related to health care and intellectual property. In response to the executive order, the Food and Drug Administration and the Department of Health and Human Services published their proposed reforms on how to handle high drug prices, putting the emphasis on intellectual property, and they do not disappoint.
Two of the three guiding principles released in the HHS report implicate the patent system for drugs:
1) Make drug prices more affordable and equitable for all consumers and throughout the health care system.
Support drug price negotiation with manufacturers and stop unreasonable price increases to ensure access to drugs that can improve health for all Americans
2) Improve and promote competition throughout the prescription drug industry
Support market changes that strengthen supply chains, promote biosimilars and generics, and increase transparency
3) Foster scientific innovation to promote better health care and improve health
Support public and private research and make sure that market incentives promote discovery of valuable and accessible new treatments, not market gaming.
There are some valid concerns about how negotiation of drug prices could impact follow-on innovation, and it’s preferable to use demand-side approaches to make newer drugs more affordable. (Notably, the HHS report does concede that “for some [new] drugs, these [high] prices might be justified by the significant clinical benefit they offer to patients.”) For older drugs, however, the rationale that high prices are necessary to spur innovation is less relevant. There are clear examples of drugs which should be off-patent but aren’t, like Humira, which have had plenty of time to recoup the costs of innovation plus a healthy return for investors. In these cases, the incentives created by the patent system have turned into excessive rents which can be trimmed through price negotiations or importation without harming innovation. This may not be the case for other drugs, and so a cautious approach is preferable.
But on questions of intellectual property and generic entry, the administration should go full steam ahead.
The HHS report, as directed by the EO, reviews legislative options to address rising drug prices. Though most of the report focuses on drug price negotiations and legislation that would control price increases, it does mention legislation which would restrict pay-for-delay deals and speed up the entry of generics and biosimilars — drugs that imitate brand-name products derived from living organisms, rather than chemical processes. That’s been sorely needed for a long time. Combined with an energetic Federal Trade Commission to enforce such laws and crack down on branded drug manufacturers who peddle doubt about the safety of generic alternatives, this approach promises to use the benefits of competition to bring down drug prices.
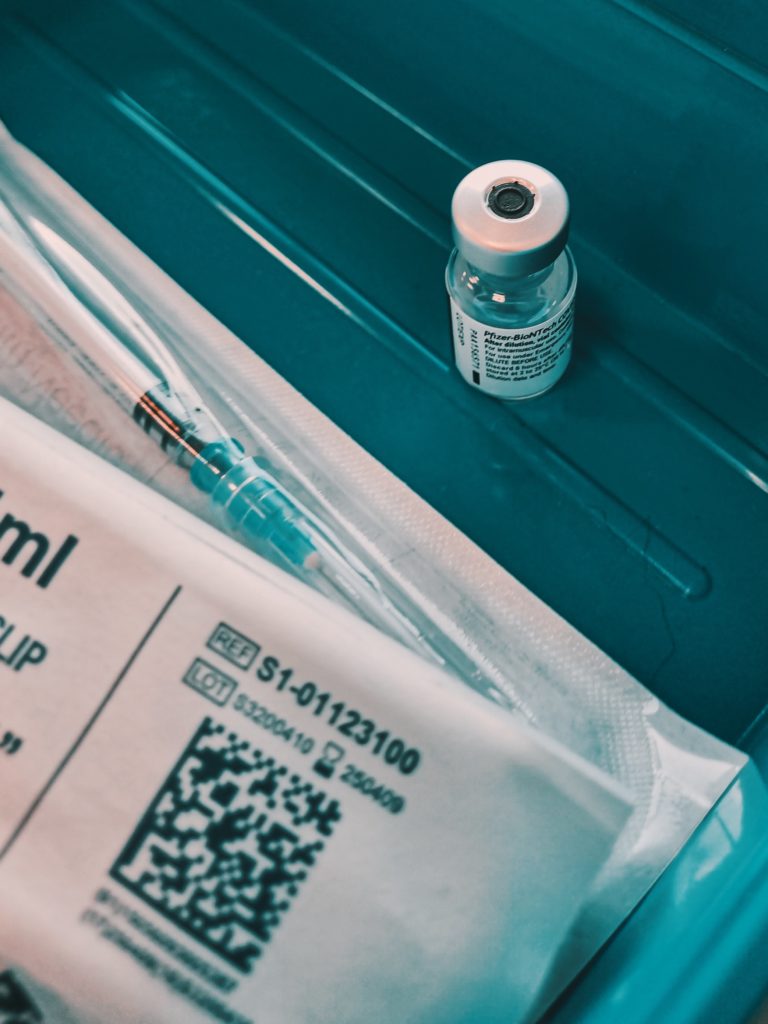
The report also discusses several potential executive actions that could help curb drug prices. One of these is accelerating the process for regulations and procedures on biosimilar and generic entry. The United States has been behind the curve on biosimilar entry and competition, but following the 2018 Biosimilars Action Plan guidance and the first-ever approval of an interchangeable biologic for insulin, Semglee, progress is finally being made. It’s also refreshing to see the administration consider “making its own review process more efficient, improving the speed and predictability of the generic drug review process while maintaining rigorous scientific standards [and b]ringing greater transparency to the generic drug review and approval process, as well as removing barriers to generic drug development and market entry, supports patients’ access to the medicines they need at affordable prices.” Following the controversial approval of Aduhelm, one might expect an administration to pump the brakes on drug entry. But generics are a very different question than the approval of new drugs, and it’s good to see that the Aduhlem controversy hasn’t poisoned conversations about speed and efficiency at the FDA.
But the most exciting consideration is the report’s discussion of compulsory licensing via the use of “march-in rights,” in which the government gives a third party the rights to use “subject inventions” developed with government support because the patent holder is not bringing it to market on acceptable terms, or the use of 28 USC 1498, which gives a broader right for the government to use or license the use of patented technologies.
This is exciting for two reasons. Should the government decide to dust off march-in rights and use it as a tool, particularly in contexts where price prevents a subject invention from achieving “practical application,” we will finally get an answer from the courts over whether or not price can serve as an impediment to such application. This has been the subject of some controversy, and while I’m firmly of the belief that march-in rights can apply to cases where price is an obstacle to access on reasonable terms, it would be good to get a definitive answer.
Second, the inclusion of Section 1498 in this discussion indicates that the administration will be more inclined to use compulsory licensing in general–not just for subject inventions under the Bayh-Dole Act–but as a cudgel against firms abusing their patent rights. Skepticism about the use of jawboning is warranted, but credible threats of compulsory licensing have been successful in the past and there’s a world of difference between an all-caps tweet from the president and serious discussion of using a law passed by Congress for its intended use. Regardless, the administration is making it clear that it is unafraid to use those tools.
The next major statement related to the competition EO comes from the Food and Drug Administration in a letter sent to Andrew Hirshfeld, acting director of the U.S. Patent and Trademark Office. It homes in on the issue of patent quality — that is, making sure patents protect truly novel inventions and are not used for “evergreening” (the extension of patent duration beyond the intended 20-year terms through practices like product-hopping and patent thicketing).
To that end, it looks at four issues where the work of the FDA and the USPTO intersect. These are:
- Giving USPTO’s patent examiners access to FDA data to help determine the novelty of a new drug;
- Examining potential misuse of the patent system to extend legal exclusivity beyond the traditional 20-year terms;
- Giving greater time and resources to patent examiners; and
- The effect of Post Grant Reviews (PGRs) and Inter Partes Reviews (IPRs), which review the validity of patents which may have been granted in error, on patents covered by the FDA’s Orange and Purple books listing approved drug and biologic formulations.
The FDA’s letter is buttressed by one from Senators Patrick Leahy (D-VT) and Thom Tillis (R-NC), the chair and ranking member, respectively, of the Senate Judiciary Intellectual Property Subcommittee. They urge Hirshfeld to crack down on drug makers trying to pass of tweaks and marginal changes to drugs as new inventions. The problem is that it’s very easy to pull a fast one on the USPTO by pitching a reformulation of a drug as a new invention while at the same time assuring the FDA that the change in formulation is unremarkable and does not require a new drug application. The tension between those two positions is obvious and borders on fraud.
To see how this works, consider the machinations of Purdue Pharma, which became infamous in the opioid crisis. The original patent for its widely abused drug OxyContin was supposed to expire in 2013. Purdue was granted a patent on what it claimed was an abuse-resistant reformulation of the drug and successfully asked the FDA to remove the original formulation from the market, blocking generic entry. It later became clear that the abuse-resistant formulation has been less than successful and transparency from the FDA has been lacking. In short, Purdue applied for a patent and extended its legal monopoly based on a false claim that the drug was abuse-resistant in a coup of regulatory gamesmanship.
That’s the tip of a very large iceberg of patent dysfunction getting in the way of drug affordability, and it’s exciting to see both the executive and the legislative branches getting serious about breaking it.