This piece was originally published by The Milken Institute Review on Jan 24, 2021.
Americans are inclined to believe they live in the land of freemarket health care. Yet the reality is that the humongous health care system (with annual expenditures close to $4 trillion) is tangled in a web of professional licensing regulations that go far beyond what can credibly be defended as advancing health. The evidence suggests that licensing damages the system in myriad ways, raising prices, lowering productivity and reducing access to care. None of this is inevitable, even in as complex a system as U.S. health care. Indeed, the streamlined licensing model common in Europe — particularly in Scandinavia — offers clues for reforming licensing in the United States without sacrificing quality or safety.
First Things First
Occupational licensing — what amounts to mandatory preapproval to work in a given occupation — is a defining feature of U.S. health care. License requirements cover the vast majority of skilled health care workers, from physicians all the way down to the most junior and entry-level roles, as well as various specialized medical equipment technicians.
Licenses confer two sorts of rights upon their possessors. First, the legal right to call oneself by a particular professional title, such as “physician” or “registered nurse.” Second, the tasks permitted a given occupation, aka the “scope of practice.”
The continuous growth of this thicket of restrictions has largely gone unnoticed by consumers. Policy researchers, on the other hand, are aware of the trend, but divided along two contrasting perspectives on what is driving the growth. The first — the “asymmetric information” hypothesis — concludes that licensing addresses the reality that consumers rarely know enough to judge the quality of health care service providers. Licensing makes it unnecessary for consumers to be experts by restricting the practice of medicine and all the subspecialties that support it to those who have demonstrated competence. This rationale is intuitively appealing and is particularly popular among members of the licensed professions themselves.
The second perspective — the rent-seeking hypothesis — concludes that licensing does not solve a problem but exacerbates one. Licensing boards, in this view, are akin to medieval guilds and exist primarily to protect their professions from would-be competitors.
That does not mean licensees always put their own interests above society’s. For instance, physicians may support the American Medical Association’s opposition to allowing pharmacists to vaccinate children because they truly believe only licensed physicians can safely carry out the task.
What matters, of course, is what the actual impact is — whether licenses benefit an interest group at the public’s expense while failing to correct a market failure suggested by asymmetric information.
What’s indisputable here is that consumers pay higher prices for the services of licensed workers, and that the workers are generally better paid and have more secure employment. These facts are consistent with either view of the function of licensing. But research largely ends up on the rent-seeking side. Evidence supporting the asymmetric information explanation is largely limited to the initial licensure of doctors and midwives during the late 19th and early 20th centuries, which probably did lead to quality improvements, including lower mortality rates. Contemporary studies, though, find that the impact of licensing on quality is small or, more often, nonexistent.
Practitioners in states that are especially stringent on licensing charge more without delivering better quality. And while the asymmetric information hypothesis predicts that increased consumer confidence translates into higher demand for services, we do not observe evidence of that, either. Indeed, as the rentseeking hypothesis predicts, studies conclude that occupational licensing generally reduces employment, sometimes substantially.
Over the past few decades, states desperate to contain medical inflation have experimented with allowing nurses into domains previously monopolized by physicians. Physician associations and licensing boards oppose these experiments, citing concerns about reduced quality. Yet there is no evidence of deteriorating quality in states that have expanded nurses’ scope of practice. On the contrary: in some cases quality has actually gone up. Furthermore, the increase in the availability of services after liberalization is generally found to translate into substantial public health benefits.
While we cannot say that licensing is never warranted by the asymmetric information problem, economists generally agree that the current licensing regime for health care professions is much too strict and adds considerably to the cost of care. Look across the Atlantic, and one finds numerous health systems with more liberal licensing regulations but with quality rivaling, if not surpassing, that of the United States.
Us Versus Them
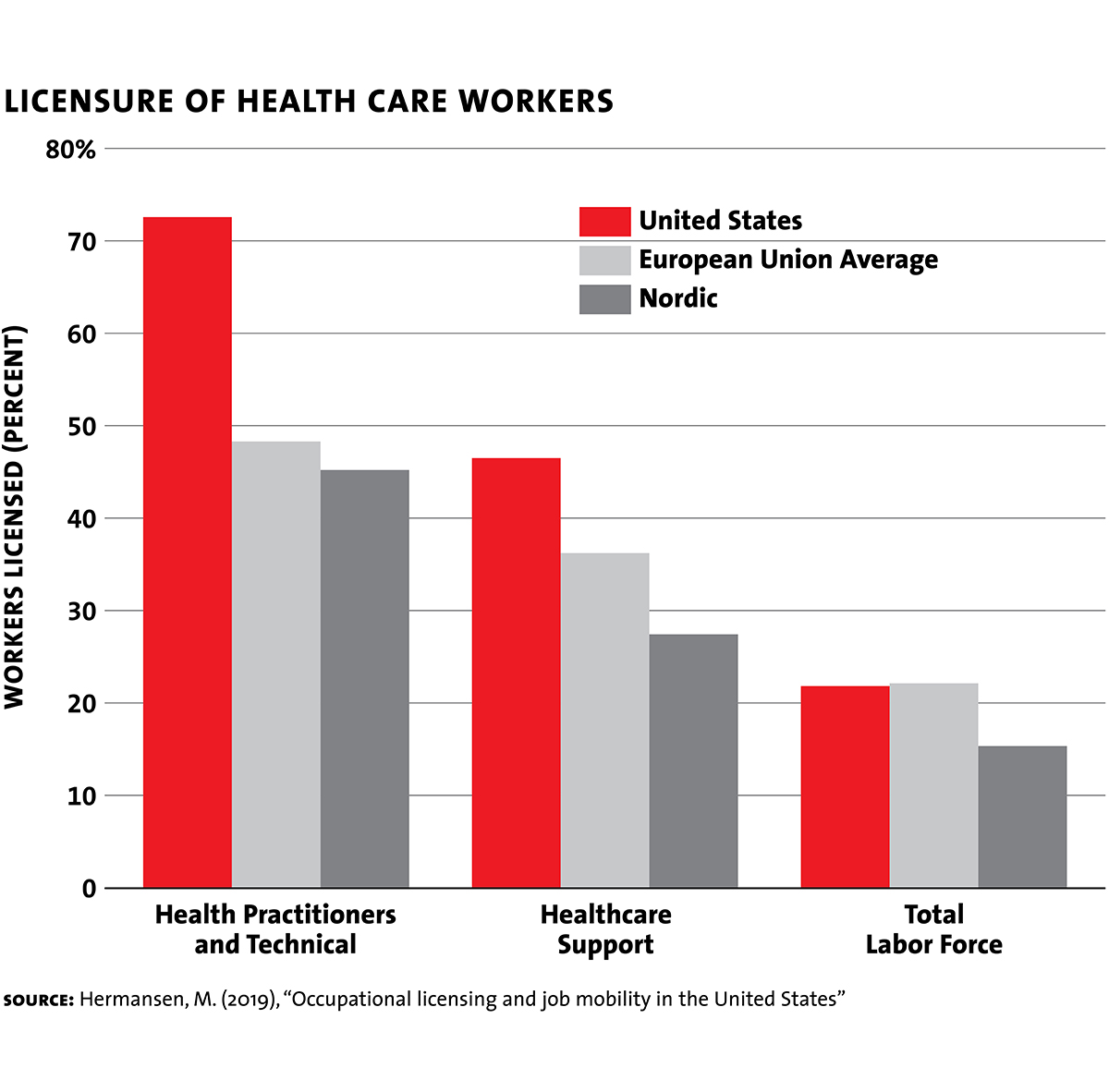
International comparisons reveal that the U.S. is a startling outlier among countries that aim to deliver state of the art care. While Europe is no stranger to occupational licensing — the EU and the U.S. require licenses of approximately the same proportion of the economywide workforce — health care is the big exception.
Today, license requirements for U.S. health care workers stretch all the way down to junior-level support occupations — positions with the titles of “technician,” “assistant” or “aide.” For instance, not only do we now license physical therapists, but many states also require physical therapy assistants and physical therapy aides to be licensed. And typically, the requirements include at least a twoyear college associate’s degree and accreditation from a third-party certifier.
Note that the expansion of licensing into these roles makes little sense even if one believes patients have no way to assess competence. Health care consumers do not choose a practitioner’s support staff, and (typically licensed) employers are more than qualified to judge whether support staff are up to snuff.
The European health care sector does make use of third-party certification for workers performing some duties. But Europeans have decided that a certification does not have to be backed up with a license, and that it’s often preferable for workers to be trained on the job rather than go through state-sanctioned third-party education programs. As such, the entry- and mid-level health providers who form the backbone of health systems across Europe typically avoid much of the hassle that dogs their American counterparts.
The EU and Scandinavia are hardly casual about job qualifications. But by largely limiting licensure to independent practitioners who directly interface with patients, European countries limit the downsides of licensing while ensuring quality. And by any objective measure, they do deliver.
Laissez-Faire Scandinavia?
European countries not only require licenses for fewer health care occupations, but their licensing regulations tend to be less prescriptive. As mentioned previously, a license can prescribe behavior in two areas: the right to call oneself by a specific professional title, and the scope of practice permitted. The United States does far more of the latter, micromanaging the tasks that health care professionals can do.
Sweden serves as a useful illustration of what a lighter touch to licensing looks like. While some tasks, like prescribing medicine, may be performed only by members of specified professional categories, the delegation of most health care tasks is largely left up to managers and supervisors. Swedish health care workers require no license to fill a tooth cavity, to operate an X-ray machine (or interpret the results), to insert a urinary catheter or to take blood samples, to name a few examples.
In the U.S., by contrast, simple tasks often cannot be legally performed even by individuals with entry- or mid-level licenses. This is because each designated specialty is heavily circumscribed by the licensed scope of practice. Adding to the crazy quilt, rules vary considerably by state. For example, a nurse assistant in Oregon may dress wounds, insert a urinary catheter and manage medical records, while nurse assistants in neighboring California may not do any of these things.
Collecting the Tolls
Where professions are licensed both in Europe and the United States, the U.S. licensure process is typically more burdensome. Fees are higher, and the administrative maze is more tortuous. Thus, not only does the American approach create higher barriers to entry, it is also a massive nuisance for health professionals already inside the tent.
Actually, this burden can be more than a nuisance. Health care workers looking to practice in other states often confront confusing, time-consuming and expensive requirements to get from here to there. Occasionally, these requirements tip from the category of frustrating to absurd. For example, dental hygienists who wish to work in Maryland, Oklahoma, Louisiana, Minnesota and Maine must sit for an in-person interview with the relevant state dental board.
Licensure processes are substantially more streamlined in Europe, typically requiring only basic documentation: proof of identity and credentials.
Fees are generally lower, too, especially in Nordic countries. In Sweden, physicians pay a one-time fee roughly equivalent to $300. In Denmark, physicians do not pay any fee at all for a basic license. An American physician, by contrast, needs to file for renewal every few years and pay hundreds or, in some states, thousands of dollars.
Federalism Gone Wild
The highly fractured nature of U.S. health care licensing compounds these costs. Unlike the licenses issued to health care workers in Europe, U.S. licenses are not valid throughout the whole country. So, a physician licensed in Maryland must apply to Virginia’s medical board to practice across the state border. This system creates barriers both to the movement of health care workers and, in some cases, to the adoption of cost-saving innovations.
Health professionals who move or simply want to work in other states must not only undergo additional rounds of scrutiny, but also pay fees assessed by both the new and previous boards. Often, the requirements imposed by state boards amount to arbitrary hurdles for those trained elsewhere. New York, for example, mandates that nurses qualified outside the state must complete specialized coursework on child abuse prevention through one of the state’s accredited providers. Given all this, it shouldn’t be a surprise that workers in licensed occupations are, on average, 20 percent less likely to move across state lines.
The need to purchase multiple licenses to practice health care is a burden that is almost unique to the U.S. It’s not a small problem: 22 percent of physicians are licensed in at least two U.S. states, and 7 percent maintain licenses in three or more. Physician licensure throughout the entire U.S. would cost well over $10,000 in renewal fees every few years. Fun fact: only 14 doctors are licensed in all 50 states.
Fractured licensing regimes don’t just create headaches for workers who change residence, but can be barriers to signing on with employers just miles away. The Philadelphia metropolitan region, for example, straddles four states. The licensing-related administrative obstacles faced by health workers there in switching employers would be unthinkable almost anywhere else in the developed world.
Many states found these barriers were unworkable in the midst of the Covid-19 pandemic and temporarily lifted them, using emergency powers. Yet there is every reason to believe these restrictions are harmful in normal times, too.
The fractured nature of U.S. health care licensing also generates substantial barriers to the emerging field of telemedicine, threatening to prevent location-blind online medical care from reaching its potential. The increased hassle and expense of multistate licensure deters telemedicine providers from offering nationwide services. Even Germany, which is the most heavily licensed country in Europe, does not have such extreme barriers to nationally comprehensive telemedicine. Instead, Germany’s location-based license requirements are tied to a practitioner’s residence rather than where they practice.
Foxes in the Henhouse
Licensing via industry-controlled state boards is always problematic, since acting as a gatekeeper in one’s own profession introduces inherent conflicts of interest.
In the United States, each state charters boards responsible for each licensed profession, such as a medical board for physicians, a dental board for dentists, and so on. The composition of these boards is statutorily determined and is generally limited to active members of the profession.
This setup is roughly akin to requiring the Commodity Futures Trading Commission to be run by active options traders. Medicine, like financial services, is a complicated business — but that doesn’t mean we ought to defer to the professionals being regulated.
By contrast, European countries have generally moved toward consolidated licensure of doctors, nurses and other health professionals under the control of government agencies. For instance, the Danish Health Authority operates under the aegis of the country’s ministry of health. (This wasn’t always the case, by the way: a century ago, all of Europe licensed much the way we still do in the United States.)
Even countries that retain professionspecific boards have gradually strengthened their independence from the practitioners they regulate. Since 2003, for example, only half the members of Britain’s General Medical Council, which oversees physician licensure, may themselves be registered physicians.
To the extent that U.S. boards incorporate representation from outside their professions, it is limited to a marginal share of the seats. Yet these boards act not only as gatekeepers, but also as intrusive lobbyists for their professions, routinely proposing legislation to serve their licensees.
Lobbying actually appears to be one of the main drivers behind the proliferation of new licenses within health care. To illustrate, Maryland’s Board of Physicians persuaded the legislature to allow it to license physician’s assistants, athletic trainers and respiratory therapists. Polysomnographic technologists — operators of diagnostic equipment used in sleep studies — are now also on board as a consequence of legislation initiated in 2013 by Maryland’s Board of Physicians. By no coincidence, each licensed occupation becomes a new source of revenue for the regulators
The reliance on fee revenue speaks to a deeper issue with the way licensing boards are structured in the United States. In being selffinancing, state boards often lack the money to meaningfully oversee their professions. Indeed, many boards have only enough funding to process paperwork and to operate a database of their members. One dangerous consequence: medical boards, in particular, are either unwilling or too understaffed to rescind licenses for even the most egregious misconduct.
Truth be told, both the United States and Europe primarily rely upon mechanisms apart from licensing to ensure health care quality, including malpractice lawsuits and inspections of facilities by other agencies. But if there is to be a constructive role for licensing to play in the United States, it isn’t going to be possible as long as medical boards are hobbled by conflicts of interest and starved of resources.
Emulate Europe
Europe offers a solid model of what to aim for. First, we should license fewer junior and technician roles. Often, these licenses simply serve as redundant hurdles imposed on top of third-party certifications. They create barriers to entry that serve no one’s interest except, perhaps, those of incumbent licensees eager to avoid competitive entry.
Ideally, a push for less licensing would be accompanied by a broader re-examination of our overbearing regulation of scope of practice. There’s every reason to believe that giving medical personnel greater leeway (under supervision) to adapt to changing demand and technology would reduce costs without reducing quality.
Second, to reduce the effects of licensing on job mobility, states should pursue deeper integration through interstate license compacts. Such compacts already help to varying degrees. Some, such as the Nurse Licensure Compact, create a genuine free-trade zone in 30-plus states, allowing nurses licensed in, say, Colorado, to work in Virginia or any other member state without additional hassle. Other compacts, such as the Interstate Medical Licensure Compact covering physicians, merely streamline the licensing process while leaving intact the need to obtain multiple licenses in order to practice in multiple states.
These compacts are limited by the reality that many states aren’t included. Moreover, many health care professionals, such as physician assistants (who are becoming increasing vital in primary care), lack any way to shorten the multistate license gauntlet.
The most significant barrier to broader compacts is political. State boards, reliant on fees from license applicants for income, stand to lose out by recognizing out-of-state licenses. Physician medical boards alone collect on the order of $350 million a year nationwide. Indeed, the very limited reach of the current compact for physicians is a reflection of how state boards function as powerful interest groups apart from the professions they regulate.
And while licensing compacts are often popular among practicing professionals, this isn’t always the case. For instance, a backlash among Rhode Island nurses over increased competition from out-of-state nurses led the state to exit the compact after more than a decade of membership.
The difficulty in achieving progress on interstate mobility speaks to the deeper issue of organizing licensing around boards dominated by the professions that they are supposed to be regulating. This arrangement is both inherently inefficient and encourages rent-seeking. To make licensing work as well as it does in countries like Denmark or Sweden, we ought to consider federal pre-emption.
One option here would be for Washington to require states to recognize each other’s licenses, allowing health care professions to move freely. This is fully within the federal government’s power, having mandated the establishment of new licenses by states in the past. It’s also clearly within the bounds of a conservative reading of the Constitution’s commerce clause. We don’t allow states to impose import tariffs on goods and services crossing the border. The same should be true with regard to barriers to trade in life-saving health care services.
A more ambitious approach would shift licensing to the federal level. This would emulate the consolidated agency model adopted in much of Europe. The key advantage would be to move beyond the soft corruption and inefficiencies associated with state boards. Most of what licensing boards actually do involves processing paperwork and managing databases, and there are obvious economies of scale to be had through consolidation.
A nationwide licensing framework would also allow requirements to be tailored around national priorities rather than the parochial interests of the professions. Consider that state medical boards effectively have the final say regarding our nation’s immigration policy for physicians. Graduates of foreign medical schools face extraordinary barriers to licensing in many states, and it’s virtually impossible for an accomplished physician from countries with high health care standards like Australia or Britain to become licensed in the United States without going through redundant residency training.
While affluent metros in the United States generally have plenty of doctors, there are growing shortages in rural areas and in subspecialties like family medicine and gerontology. A national licensing system would make it far easier for foreign doctors to establish medical practices where demand is high. Last, but not least, a system in which licenses are issued by an independent taxpayer-funded agency would remove the revenue imperative that leads state boards to lobby for wasteful regulations in the first place.
• • •
The ironies here are glaring. Americans, steeped in the mythology of free-market fundamentalism, love to contrast home-grown efficiency with the economic arteriosclerosis that is allegedly the fate of the European welfare states. Yet in the case of health care credentialing, Europe is far ahead in streamlining regulation without undermining quality. We need to swallow our pride and acknowledge that American particularism isn’t always a good thing.